A strong dollar and high US rates have frozen the world, says El-Erian
Policymakers around the world are facing challenges from a strong US dollar and high interest rates, as noted by Mohamed El-Erian, president of Queens College, Cambridge. He noted that authorities…
Premier Tech and MG Tech collaborate on packaging technology
Premier Tech and MG Tech have joined forces in a strategic partnership to address the changing needs of manufacturers across industries including food, industrial, consumer goods and parapharma. By combining…
Nearly $660 million in bets placed during the inaugural month of sports betting
North Carolina officially legalized sports gambling on March 11th, and since then, state residents have placed nearly $660 million in bets between March 11th and March 31st. This amount includes…
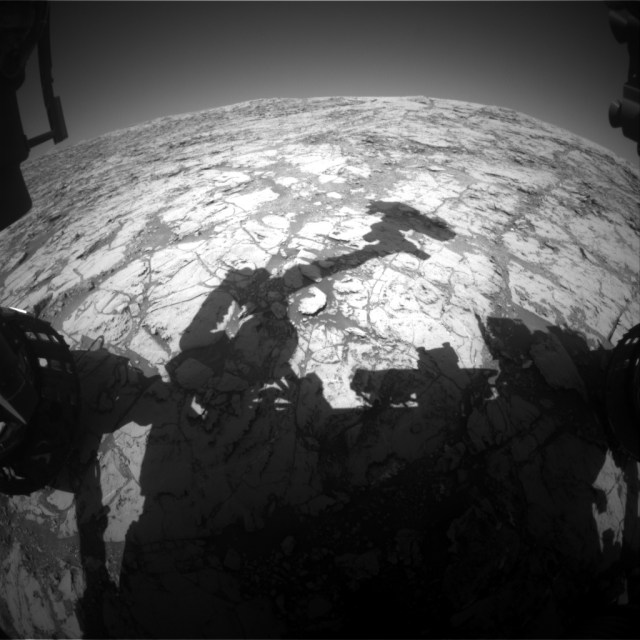
Here we go again: deja vu
After we thought we were finally leaving our current spot on Mars, a mistake during one of our arm activities resulted in us staying one more sol. This setback caused…
USU Continuing Education Emphasis: “Exploring Mental Health Conversations for Coal Miners”
The HEART Initiative at Utah State University, along with the Southeastern Utah Department of Health, will host a conference called “Conversations for Coal Miners and Mental Health” on Tuesday, April…
Challenges facing the US in ending economic support to Iran
After Iran's recent attack on Israel, analysts say the US faces challenges in tightening sanctions on Iranian oil amid concerns over rising oil prices and strained relations with China. The…
The Ishpeming Rotary Club is bringing back the Westwood Business Professionals of America
The Rotary Club of Ishpeming has generously donated $500 to support Westwood High School students as they prepare to attend the BPA National Leadership Conference in Chicago in May. The…
Israel appreciates the EU's commitment to enforcing sanctions against Iran
Israel celebrated the European Union's commitment to imposing sanctions on Iran following Iran's recent drone and missile attack following the Israeli bombing of the Iranian consulate in Damascus in April.…
The largest gold block in the world
In February 1869, two British prospectors, John Deason and Richard Oates, made a historic discovery in central Victoria, Australia. While digging for gold, they came across a large rock which…
Thelin sees Aberdeen as 'perfect match'
Jimmy Thelin, who is currently coaching Elfsborg in the new Allsvenskan season, has expressed his excitement at the opportunity to manage Aberdeen from the summer. Thelin, a 46-year-old Swede, believes…