Rebuilding Together: Tkuma Directorate Announces $1.5 Billion for West Negev Settlements Reconstruction following Devastating Attacks
In response to the recent attacks on West Negev settlements, the Tkuma Directorate has announced a project to rebuild the affected communities. The ten hardest-hit settlements will receive NIS 1.5…
From Adversity to Triumph: A Virtual Panel Discussion on National Small Business Week and the Story of Selma’s Award-Winning Small Business Owner Jackie Smith
On Monday, April 29 at 3:00 PM CDT, U.S. Representative Terri Sewell of Alabama’s 7th District will host a virtual panel discussion to kick off National Small Business Week. The…
China Takes a Stand for Palestine: Supporting Unity Government with Hamas and Promoting Peace in the Region
The Chinese government has shown its support for the Palestinian Authority in its efforts to form a unity government with Hamas, despite years of conflict between the two groups. This…
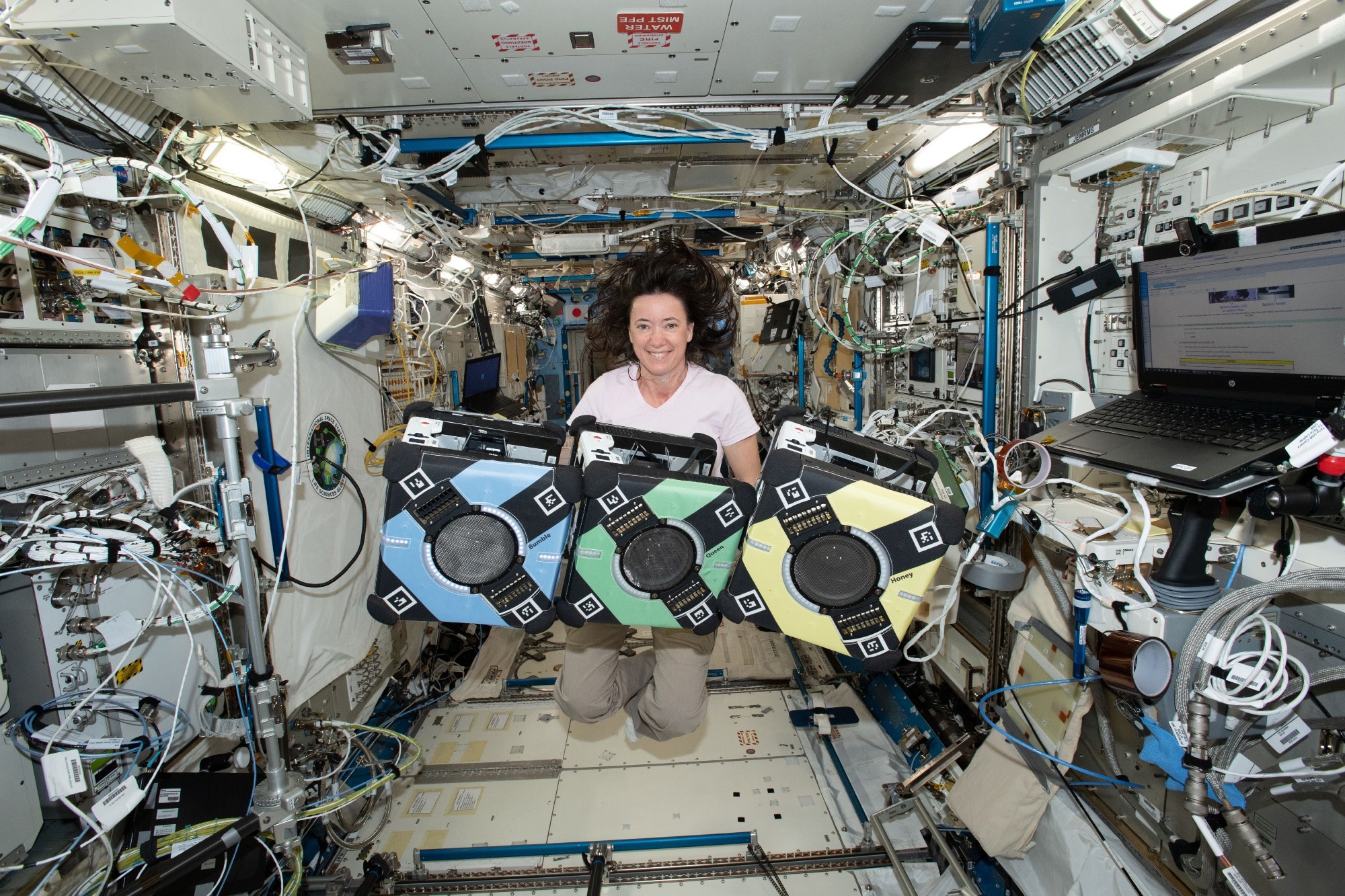
Revolutionizing Space: The Impact of Astrobays on Scientific Research and Future Spaceflight Missions
Astrobays, NASA’s trio of free-flying robots, are making waves in the scientific community as they assist astronauts and conduct valuable research on the International Space Station (ISS). In the latest…
Nj High School Game Changers Sports Awards 2024: Recognizing Positive Impact on Teams, Schools and Communities
The second annual Nj High School Game Changers Sports Awards are now open for voting. To cast your vote, simply scroll to the bottom of this article where you’ll find…
Outstanding Achievements Recognized: Super Science Club and Adventure Society Receive Impact and Excellence Awards
The Impact and Excellence Awards recognized the outstanding contributions of over 50 students, faculty, and staff to the College community. Among them, the Super Science Club was awarded Outstanding Club…
How to Access and Change Your Health Records with MyWellSpan: A Guide
Individuals have the right to access and request changes to their health records under the Health Insurance Portability and Security Act (HIPAA). MyWellSpan is a convenient way for users to…
Kauppalehti Launches Innovative Election Machine for European Parliament Candidates: Helping Voters Choose Wisely
The European Parliament election is fast approaching, and voters in Finland are gearing up to make their voices heard. To help them choose the right candidate, Kauppalehti has launched an…
NFL Draft Boosts Local Businesses: Sauced and Local Pig Pigwich Share Insights on the Unpredictable Nature of Major Events
In 2023, Union Station in Kansas City played host to the NFL Draft, providing local businesses with an unparalleled opportunity to experience the excitement firsthand. Jaiaun Smith, owner of Sauced,…
BCHS Odyssey of the Mind Team Scores Second at New York State Finals, Earns Spot at World Championships
The Bethlehem Central High School Odyssey of the Mind team has achieved a remarkable feat by placing 2nd at the New York State Odyssey Finals in Syracuse. This exceptional team,…